Various methods are used in cancer diagnostics, but the only way to finally confirm the diagnosis of a malignant tumour is to perform the pathologic examination of the biopsied material. In this article we will discuss how the tissue is obtained in the biopsy process, how it is examined, and items a patient should expect to find in the final pathology report.
In one of the previous articles (link), we discussed the process of cancer diagnosis and the methods that are used in it. This is a multi-stage process and is influenced by symptoms and the general health of a given patient. Invariably, however, regardless of the results of imaging and laboratory tests, in order to confirm the diagnosis of cancer, it is necessary to collect cancer cells or tissues and the specimen needs to be examined under a microscope by a specialist in this field, i.e., a pathologist. The final result of this process is presented in a pathology report.
How to obtain tissue for examination by a pathologist?
The process of obtaining biological material to make a diagnosis is called a biopsy. There are many types of biopsies. As a general rule, the larger the sample taken from the patient’s body, the more additional tests can be performed and the more precise diagnosis can be made, but also the greater the discomfort and risk of complications for the patient. In most cases, biopsies are primarily performed for diagnostic purposes, and not to cure the patient. Sometimes, depending on the diagnosis, the biopsy might be the only procedure that is necessary for the patient. Not every neoplasm has to be removed, especially if it is benign and does not cause any other symptoms.
A fine-needle aspiration biopsy allows the evaluation of cells and very small tissue fragments. It is a relatively minimally invasive procedure, most often performed with a needle resembling those used for injections. Very often, this method is sufficient to tell whether a given lesion is cancerous and roughly determine its histological subtype. However, due to the small amount of sampled material, it may be insufficient for an accurate diagnosis and determining the molecular profile allowing the implementation of appropriate treatment. The procedure, especially if performed on a superficially located lesions, is relatively painless and very rarely associated with any complication. Most of the patients can go home 15 minutes after the fine needle aspiration biopsy of breast or thyroid lesions. Longer hospital stay may be required for biopsies of deeper located organs, like the liver.
Bone marrow biopsy
A bone marrow biopsy is a special test used to diagnose hematopoietic system diseases such as leukaemia. During the procedure, blood is sampled directly from the location where it is produced, i.e. the inside of the bone. Additionally, sometimes the test is supplemented by removal of a bone fragment (so-called trepanobiopsy) for further testing. As this procedure may be painful, it is recommended to perform it under local anaesthesia. In most cases it can be performed in an outpatient clinic, and the patient can be discharged within an hour of the biopsy. In patients suffering from blood neoplasms, this test can be sufficient to establish a final diagnosis and initiate the treatment.
Incisional biopsy
An incisional biopsy involves collecting a fragment of the tumour. One of its subtypes is the core needle biopsy. Similarly to the fine-needle aspiration biopsy, a special needle is used to collect a sample; however, in this case it has a larger diameter, allowing the doctor to obtain larger pieces of the tissue and make an accurate diagnosis. The core needle biopsy is performed when prostate cancer is suspected, where usually a dozen or so tissue fragments are collected from strictly defined locations (so-called mapping) and more suspicious lesions visible in radiological examinations. Both fine- and core-needle biopsies can be performed under control of radiological imaging, which helps to confirm that the collected material definitely comes from the suspicious lesion.
Excisional biopsy
An excisional biopsy involves removing the entire lesion. If malignancy is suspected, the excision should also include the surrounding tissues (the so-called healthy tissue margin), because single cancer cells penetrating into healthy tissues will not be visible to the naked eye or in radiological examinations. Sometimes, in order to ensure a sufficiently wide margin, a decision is made to remove a part of an organ, the entire organ or even a group of organs. If the cancer has not spread, an excisional biopsy is often enough to cure the patient completely, provided that the excision has been made with a sufficiently wide margin – which is assessed under a microscope.
Different types of biopsies can be performed for skin lesions. In pigmented lesions that raise a suspicion of malignant neoplasm, i.e. melanoma, the excisional biopsy is preferred. In the case of other lesions, the doctor can performed a so-called punch biopsy, i.e., an incisional biopsy using a special device that removes a round piece of skin. It is also possible to remove only the superficial skin layers during the so-called shave biopsy. As with other biopsies, larger samples often give more information, but the final cosmetic effect after the procedure must also be taken into account, especially for lesions located on the face.
Endoscopic biopsy
An endoscopic biopsy is a special type of biopsy. It is carried out during an endoscopy procedure, involving inserting a thin tube with a camera into the digestive, respiratory, or urinary tract. This biopsy can either be incisional or excisional, depending on the size of the lesion.
Various body fluids, such as urine, sputum, and cerebrospinal fluid, are also subject to cytological examinations, primarily analyses and examination focusing more on cancer cells and less on tissues. Most often, however, their diagnostic value is lower than that of tissue samples, but sometimes they can be used to make a preliminary diagnosis.
How does a pathologist examine tissue?
The pathological examination consists of several phases. During the first, material is assessed with the naked eye and sections of larger lesions are taken – so called grossing. Most often, the material is evaluated within 12-72 hours of fixation in 10% formalin solution. A doctor specializing in pathology or other trained personnel examines the collected tissues and describes them according to accepted guidelines. Then, they select parts that will allow full microscopic evaluation or analyse further the entire material. The size of the sample should be large enough to allow additional tests, such as molecular analyses, if needed. Material not used during tests is stored at least until final diagnosis is made, in case additional samples are needed, and then disposed of.
The selected tissue is fixed and embedded in paraffin, to obtain paraffin blocks. Such blocks can be stored for years without losing their diagnostic value, and this is very useful, for example, when a secondary opinion is needed. In order to prepare the slides for microscopic evaluation, the blocks are cut into microscopic slices and then subjected to a complex staining process using numerous reagents. Nowadays, this process is carried out automatically. Material from cytological tests, such as a fine-needle aspiration biopsy or cytology of body fluids, is also stained. The entire process, from collecting biopsy samples to prepare slides, takes from few to several dozen hours. Then they are assessed under a microscope by a doctor – a specialist pathologist.
The so-called intraoperative consultation, or “frozen sections”, is a special type of examination. A sample taken during the surgical procedure is not fixed with chemical reagents, but frozen and immediately cut and stained. This shortens the time for obtaining microscopic slides to several minutes, but the tissues visible in them are often significantly damaged, so a definitive diagnosis is impossible. This examination is used during the surgery, to quickly determine the general nature of the lesion, if a previous biopsy was not possible, as well as to assess whether there are any cancer cells left in the patient’s body after the lesion was removed (margin examination).
Tissue examination by a pathologist step by step
A pathologist searches under a microscope for anything that looks different from normal, healthy tissues and cells. If any such area is found in the slide, they focus on cell shapes, size and patterns formed, and match them to the images of diseases known to them. When more than one disease presents a similar microscopic picture, additional tests may be used to establish the diagnosis.
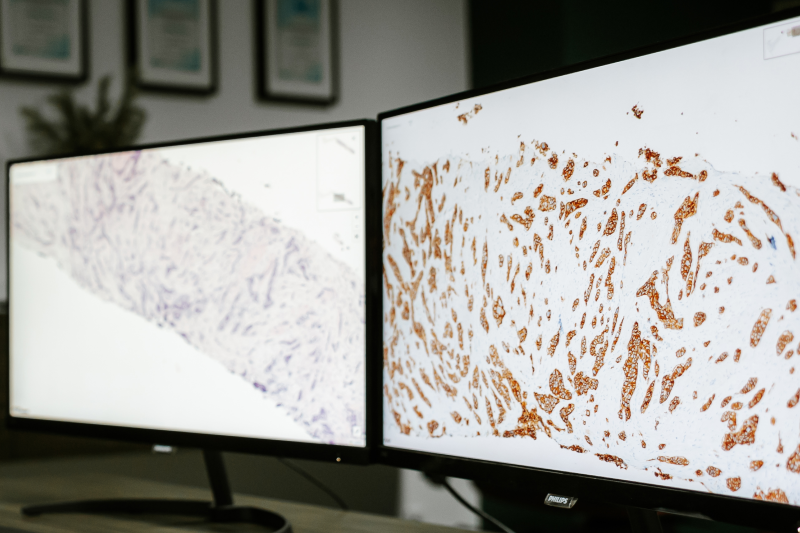
These include immunohistochemical staining to visualize specific proteins within cells, histochemical staining to reveal other chemical substances, as well as molecular pathology methods such as in situ hybridization or next-generation sequencing to search for specific genetic abnormalities. In case of excisional biopsies of tumours, the microscopic evaluation also involves examination of margins. If tumour cells are found in the margin of removed tissue, this means that some part of it was left in patients body and further treatment is usually necessary.
The pathologist’s final diagnosis is always based on available clinical information, because lesions of identical appearance may be interpreted differently in children and the elderly, or in men and women, and depending on the symptoms and other important facts from the medical history, which should be specified in a referral or otherwise available to the pathologist. The final result of the histopathological examination is always provided in form of a pathology report.
Digital pathology
Digital pathology is a sub-field of pathology, and involves the acquisition, sharing, management and evaluation of collected information. Nowadays, artificial intelligence is also used in microscopic examinations, and supports the pathologist in image assessments. For this purpose, the slides are scanned and then subjected to image analysis using specialized algorithms developed for this purpose. This method allows for additional verification of the diagnosis. In addition, scanning the slides enables laboratories to quickly share the image when a second opinion is required.
What is a pathology report?
Pathology reports are the final result of the process of evaluating the material (cells and tissues) from the biopsy. A report is usually very formal and consists of several parts. It should include a description of the collected material such as tissues, parts of organs, and tumours, a microscopic description of the assessed slides, a description of the performed additional tests, such as immunohistochemical and molecular staining, as well as the final diagnosis, which is its summary. This report should always be signed by a physician specialized in pathology.
What should be included in the pathology report?
The macroscopic description can be short, if only a small fragment of a neoplastic tumour has been collected, or very long and complex, if an entire organ or group of organs has been excised. It contains a description of all observed changes deviating from the normal appearance for a given tissue, including their characteristics such as size, consistency, colour and distance from the nearest edge (the so-called margin width). When samples are taken, they are labelled in the description, so the pathologist evaluating the slides knows the site of viewed images. If the description was drawn up by a person other than the doctor conducting the microscopic examination, their name and qualification should also be provided in the report.
The microscopic description includes all features of the assessed image that were important for the diagnosis or may impact further treatment. The description may be written as a continuous text, but increasingly often specialized surveys (so-called synoptic reports) are used for this purpose, which allow verifying whether all elements relevant to the diagnosis of a given cancer have been properly examined.
The report should also include a description of all additional tests performed, regardless of whether their results were positive or negative. This serves to prove that the examining physician took into considerations other possible diagnoses and used proper tests to exclude them. The results of additional tests are often very important for the further treatment process, allowing for the use of personalized treatment with targeted therapy. It is also worth mentioning that not every laboratory is equipped to conduct all tests required for modern diagnostic processes.
What is the diagnosis on a surgical pathology report?
The final diagnosis is a summary of the entire pathology report. Based on it, the treating physician should be able not only to learn the type and the stage of cancer that the patient is suffering from, but also to establish treatment they can potentially use.
How will I find out what is in my pathology report?
The pathology report is prepared primarily for the treating physician, but the patient should always be able to receive and verify it. If it has been prepared in the form of a synoptic report containing numerous abbreviations which might be difficult to decipher, it is advisable to ask the attending physician or the pathologist who prepared the report to help in reading and understanding it.
As we can see, the final quality of the pathology report depends on multiple factors. The proper collection and handling of tissue samples, the sufficiently equipped laboratory to conduct immunohistochemistry and molecular analyses, as well as the pathologist’s experience, knowledge and skills, all impact the final diagnosis. If there are any doubts as to the pathology report quality, the best solution is verify it by seeking a second opinion, as is crucial for further treatment choices.
Author: Adam Gorczyński, MD, PhD