The term cancer does not refer to just one illness, but covers a diverse group of diseases with a myriad of different manifestations. That is why cancer diagnostics require multiple steps and a personalized approach. In this article, we will discuss various methods that can be used in this process, with pros and cons of each of them explained.
How to diagnose cancer?
Cancer diagnostics are a complicated process, the purpose of which is to confirm the presence of a neoplastic disease, determine its stage and decide on the best possible treatment. There is no single test that can detect every type of cancer. Not without reason – as we wrote in one of the previous articles (What is cancer?), actually the term cancer does not refer to one disease, but covers a diverse group of diseases that can affect basically every tissue and cell in our body.
In the past, the cancer diagnosis was primarily based on examining the patient in the doctor’s office and discussing the symptoms. A physical examination can still be helpful in detecting superficially localized or very advanced lesions, and the first step in detecting cancer frequently involves identifying its symptoms.
Unfortunately, very often they are non-specific, i.e. they do not enable distinguishing the tumour from other diseases. Furthermore, cancers of the same organ and belonging to the same subtype can manifest with completely different symptoms in two people! Therefore, it is necessary to use other methods enabling more precise diagnosis. The progress in medicine offers new options for diagnosing cancer at an earlier stage, and thus increases the chances of curing it.
Furthermore, advances in the medical science have expanded our understanding of cancers biology, resulting in new therapies targeting specific cancer types. Nowadays, the proper diagnostics process includes conducting blood tests, radiological imaging, and a thorough examination of the tumour tissue under a microscope, as well as analysing it for genetic aberrations, which often allows the use of individualized, „tailored” targeted therapy.
What are the different types of methods or lab tests used to diagnose cancer?
Basic blood tests used in cancer diagnostics include, e.g., a complete blood count with smear evaluation. It can be used not only to diagnose blood neoplasms such as leukaemia, but also to detect anaemia, which frequently is a symptom of cancers associated with the chronic bleeding, such as colon adenocarcinoma.
Cancers very often produce all sorts of substances that can be detected in the blood. They can be the same as those produced by the tissue from which they derive, like prostate specific antigen, PSA, in prostate cancer, or completely unrelated to them, as it is the case, e.g., with adrenal hormones produced by some lung cancers. When these substances, sometimes called “tumour markers”, are detected, cancer may be suspected, but, unfortunately, they are not specific enough to become a reliable diagnostic method in themselves. However, they proved very useful in postoperative follow-up, where a sudden increase in markers usually means the disease recurrence.
Diagnostic imaging - characteristic of different types
Cancer tissues are made up of two components – the actual cancer cells and the surrounding “stroma” containing the vessels that supply them with blood and nutrients needed by a rapidly growing tumour. This structure differs from normal body tissues, therefore the tumour can be visualized in scans using ionizing radiation (X-ray, computed tomography), ultrasonic waves (ultrasound), gamma radiation (positron emission tomography), or magnetic fields (magnetic resonance imaging). With diagnostic imaging, not only cancer in the form of a tumour located inside the body can be detected, but also it can be determined whether the disease is at an early stage or is already advanced and has metastasized.
Imaging methods using ionizing radiation are the fastest and relatively cheap, providing images of high quality, but they also have their drawbacks. Too frequent exposure to them can lead to tissue damage from radiation. Additionally, some tissues, such as fibrous tissue found in breasts of younger women, are difficult to assess in an X-ray scan.
Digital Imaging
Ultrasonography represents another low-cost imaging method. It is used for the real-time assessment of tissues and organs, without causing any injury. It also allows the assessment of blood flow through a specific tissue, facilitating distinguishing between cancerous and healthy ones. Therefore, doctors often use ultrasonography as an auxiliary method when taking tissue samples (biopsy). However, ultrasonography disadvantages include a low resolution of images which does not allow for a very accurate assessment of lesions, as well as poorer penetration of ultrasound waves in some tissues (e.g. fat). Furthermore, because it is a live technique, its quality is highly dependent on the skill and experience of a doctor or a technician performing it, as post-factum consultations are impossible.
Magnetic resonance imaging is a more expensive, but safe and accurate method for examination of many organs. Therefore, it is very often used to assess if the cancer is advanced, i.e. whether it spread to other organs. Its main disadvantages are its duration, because the patient must remain still in a small tube for a long time, as well as the accompanying loud noise. Furthermore, high quality imaging of organs that are in constant motion, such as lungs, intestines or heart, is not possible.
Positron emission tomography is also used to assess the cancer spread. During the scan, the patient is administered a radioactive substance that is similar to glucose (fluorodeoxyglucose), called radiotracer, which is then visualized by a scanner equipped with gamma cameras. Cancer cells are characterised by a different metabolism when compared to healthy ones, and their demand for glucose is higher. Therefore their uptake of the tracer also is much higher, which make them visible in the image. Unfortunately, the radiation dose received during this scan is even 500 times larger than with chest X-ray and about two times higher than in the case of computed tomography. However, it is still a relatively safe dose if the patient is not exposed to other sources of radiation. Other disadvantages include lower resolution of images, and higher costs and longer time needed for the scan, when compared to other imaging methods.
What are the different types of endoscopic examinations used to diagnose cancer?
Endoscopy is a specialized examination technique for visualisation of the tumour growing, e.g. inside the large intestine (colonoscopy), stomach and oesophagus (gastroscopy), or the respiratory tract (bronchoscopy), and collecting samples from it for further examination (a so-called biopsy). For this purpose, a special thin tube equipped with a camera and other tools is inserted into the patient’s body through the mouth (gastroscopy, bronchoscopy) or rectum (colonoscopy).
A definite advantage of this procedure is the possibility of a very precise assessment of the organ potentially affected by the disease and taking samples from locations otherwise difficult to access. The obvious downside is the discomfort associated with this procedure experienced by some patients, which, however, can be alleviated with the use of anaesthesia.
Types of genetic tests used to diagnose cancer
As mentioned in the introduction, molecular testing of the tumour tissue frequently allows selection of the most effective method of therapy. Usually, material for testing comes from a collected tissue sample, and genetic testing is a part of diagnosis made by a pathologist; the process which will be discussed in detail in a separate article. However, increasingly often it is also possible to perform the so-called liquid biopsy. When the body is attacked by cancer, it is frequently possible to detect fragments of cancer cells in the blood. This is true even at the early stages of the disease, when metastases have not yet developed. This allows the genetic material of the tumour to be examined without performing a surgical biopsy.
What are the tumor biopsy variants used to diagnose cancer?
Performing a biopsy is the best way to determine whether a lesion is cancerous. It involves collecting and examining cells (a fine-needle aspiration), tissues and tumour fragments (incisional biopsy), or the entire tumour or the involved organ (excisional biopsy). As previously mentioned, it is possible to perform a biopsy (incisional, and in the case of small lesions, even excisional) during the endoscopic examination. Apart from allowing a thorough diagnostic process, excision of the entire lesion may also be a curative procedure for tumours that have not yet metastasised.
The fine-needle aspiration
The fine-needle aspiration allows the evaluation of cells and very small tissue fragments. It is a relatively minimally invasive procedure, most often performed with a needle resembling those used for injections. Very often it is a adequate method to tell whether a given lesion is cancerous, and to make a preliminary diagnosis. However, the small amount of sampled material may be insufficient for an accurate diagnosis and determining a molecular profile allowing for the implementation of appropriate treatment.
The advantages of the fine needle aspiration are that this technique is painless and very rarely results in complications. In most cases, the patient can go home 15 minutes after the puncture of superficial organs, such as the thyroid gland or breast. Longer follow-up may be required in the case of biopsies of deeper organs.
Bone marrow biopsy
A bone marrow biopsy is a special test used to diagnose hematopoietic system diseases (e.g. leukaemia). For this purpose, blood is sampled directly from the place where it is produced, i.e. the inside of the bone. Additionally, sometimes the test is supplemented by collecting a bone sample (so-called trepanobiopsy). It is performed under local anaesthesia because this is a painful technique. In patients suffering from blood cancers, this test may be sufficient for initiating treatment.
Core needle biopsy, incisional biopsy and excisional biopsy
Biopsies in which tissue material is obtained (core needle biopsy, incisional biopsy, excisional biopsy) allow determining the nature and specific type of cancer, as well as performing precise molecular tests. The effective diagnosis based on the biopsy requires material of good quality and in appropriate quantity. The larger the fragment collected, the greater the chance of making an accurate diagnosis, but also the greater the chance of potential complications after the procedure.
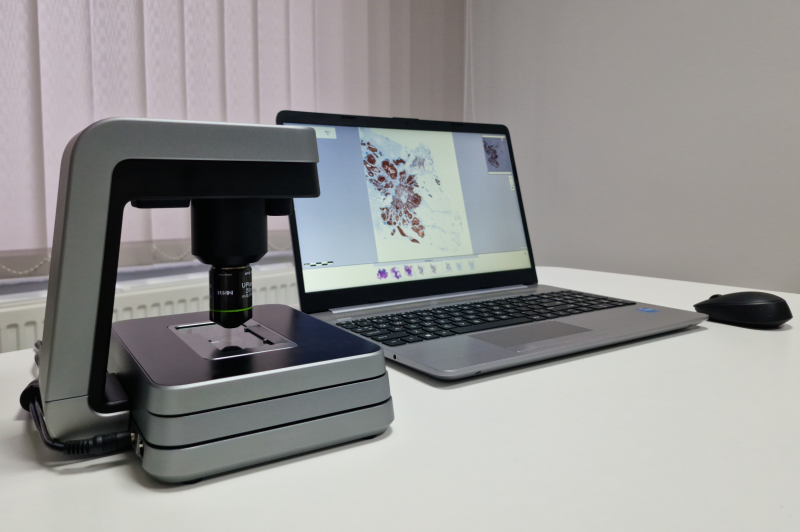
After collection, the biopsy material is subjected to specialized processing to create microscopic slides and enable its long-term storage. Modern laboratories also scan images and store them on servers, enabling the use of artificial intelligence technologies as an auxiliary procedure in making the diagnosis. It is also useful for fast consultations on difficult cases and getting second opinions when a patient wishes to receive one.
Summary
As we can see, nowadays, the diagnosis is a multi-stage, complicated and time consuming process. The selection of appropriate tools and diagnostic methods depends on the clinical picture, availability of a specific hospital or laboratory, as well as doctors preferences. However, the tumour biopsy is the procedure that has to be used always to confirm that the patient suffers from cancer.